Medical Billing and Credentialing
What is Medical Billing?
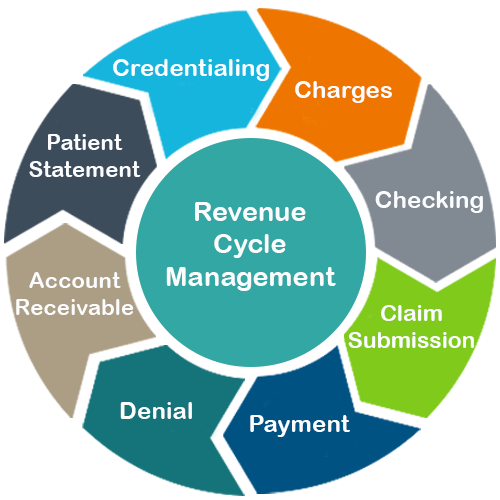
Medical billing is the process of submitting and following up on claims with health insurance companies in order to receive payment for services rendered by a healthcare provider. Medical billing process is also called as RCM (Revenue Cycle Management) workflow. It consists of nine steps starting with Credentialing/Enrollment, Coding, Charges, Checking, Claim submission, Payment posting, Denial management, Follow up/Account receivable and Patient statement.
What is Credentialing and Contracting?
Provider credentialing is the process of getting a physician or a provider affiliated with the payers. It is critical step in Revenue Cycle Management which involves a lot of manual work in terms of completing the application forms, providing clarifications to questions from the payers and following up to complete the credentialing. ABCLLC focus on getting the provider enrolled quickly to eliminate any delays in payment. Our goal is to simplify the process and reduce the cost. Our team will manage the credentialing process from the start to end of the applications.
- NPI registration (Type I and Type II)
- Medicare (PECOS) and Medicaid credentialing
- Managed care credentialing (Medicare and Medicaid)
- Commercial insurance credentialing
- Follow up with the insurance payers until the final credentialing approval
- Re-credentialing with all the payers
- CAQH profile creation, maintenance, and re-attestation.
- Hospital PHO/IPA applications.
- Payer fee contract negotiation.
- Medical license and DEA renewals.