Charge Capture Services
Charge Capture Services
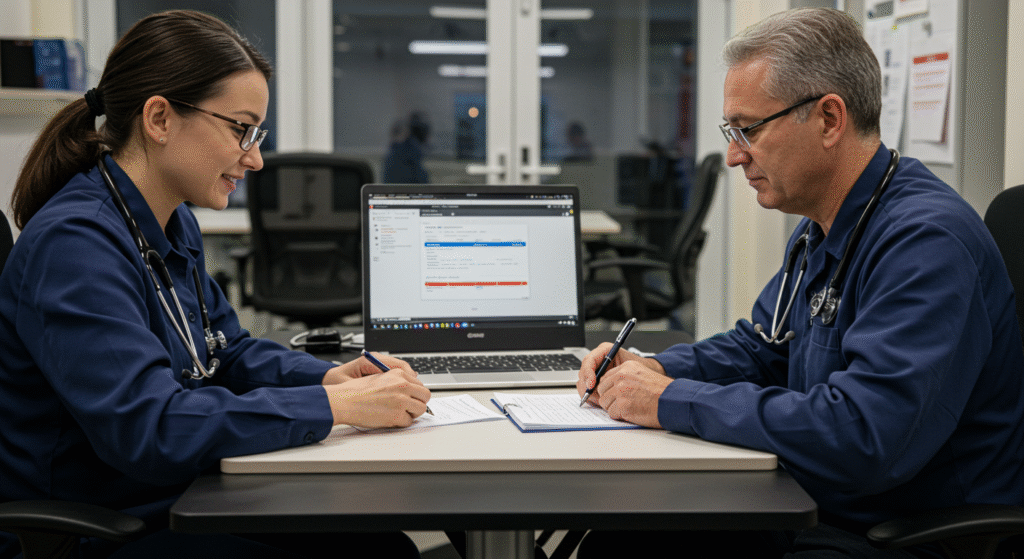
Charge capture plays a crucial role in Medical billing. Charge capture or charge entry is a process of creating a claim for a service rendered by the provider to the patient. A claim is the most important aspect for getting reimbursements. Even a minor mistake in charge capture impacts the entire outcome. ABC gives high importance for accurate charge posting in order to submit clean claims.
Benefits & Goal
ABC’s goal is to get paid at the very first submission and the team relentlessly pushes harder to achieve a higher first–pass rate of claims. We are experienced in various Practice Management Systems and various medical specialties. We have predefined rules in charge entry for different medical specialties, which reduces the room for errors and contributes to clean claims.
Charges entry includes the following:
- 1. Charge or Superbill files posting
- 2. Patient demographics entry and verification
- 3. Patient eligibility verification
- 4. Claims creation
- 5. Missing charges reminders
We also ensure:
File Handling & Reminders
ABCLLC will download the charge entry files from several file sharing applications such as Dropbox, Google Drive, PMS, FTP, Email, Fax etc. If the client prefers ABC will train them to upload the files in their own practice management system.
- 1. Charge or Superbill files posting
- 2. Patient demographics entry and verification
- 3. Patient eligibility verification
- 4. Claims creation
- 5. Missing charges reminders
Patient demo entry, data and eligibility verification
- All new patients information such as patient, guarantor, Insurance information are entered
- All existing patient information is verified and updated
- All non-office patients, demographics verified by logging into hospital or facilities portal
- ABC verifies patients insurance ID, name, address of the insurance, group name, group number, effective date, termination date, the name of the insured, date of birth and the relationship of the insured to the patient
- ABC verifies coverage for primary, secondary and tertiary payers by utilizing payer websites, automated voice response systems and calling
- All self-pay and indigent patients are checked for Medicaid and other possible insurances eligibility
Claims creation
All the claims were posted and created in 8 hours
- Charges are entered in PMS based on specialty specific CPTs and ICD 10 rules
- Handwritten diagnosis and procedures are analyzed to find the appropriate ICD-10 and CPTs
- Handwritten hospital patients’ diagnosis are cross checked with the patients progress notes by logging into the hospital portal for accuracy
- Using appropriate modifiers, mapping, linking CPT and ICD 10 codes etc., to avoid denials
- Educating providers of any obsolete or deleted CPT’s
- Precertification numbers for non-office patients are requested through fax and calling the facility before the claim is created
- Email request to the practices regarding missing Diagnosis, CPTs, DOS, etc.
Missing charges reminder
It is very important to submit claims to the insurance within the filing time limit period. Delay in the charge entry directly impacts the reimbursements.
- Weekly reminders to the provider regarding missing charges
- Weekly reminders to providers on incomplete office progress notes.