Payment Posting In Medical Billing
Accuracy in payment posting in medical billing is imperative for an optimized revenue cycle. Once payments are posted to patient accounts each denial is addressed separately. Rejected claims, late payments, and untimely patient statement submission can eventually lead to a huge loss for healthcare practices. ABC handles the payment posting in medical billing according to client-specific rules that would indicate the cut-off levels to make adjustments, write-offs, refund rules, etc.
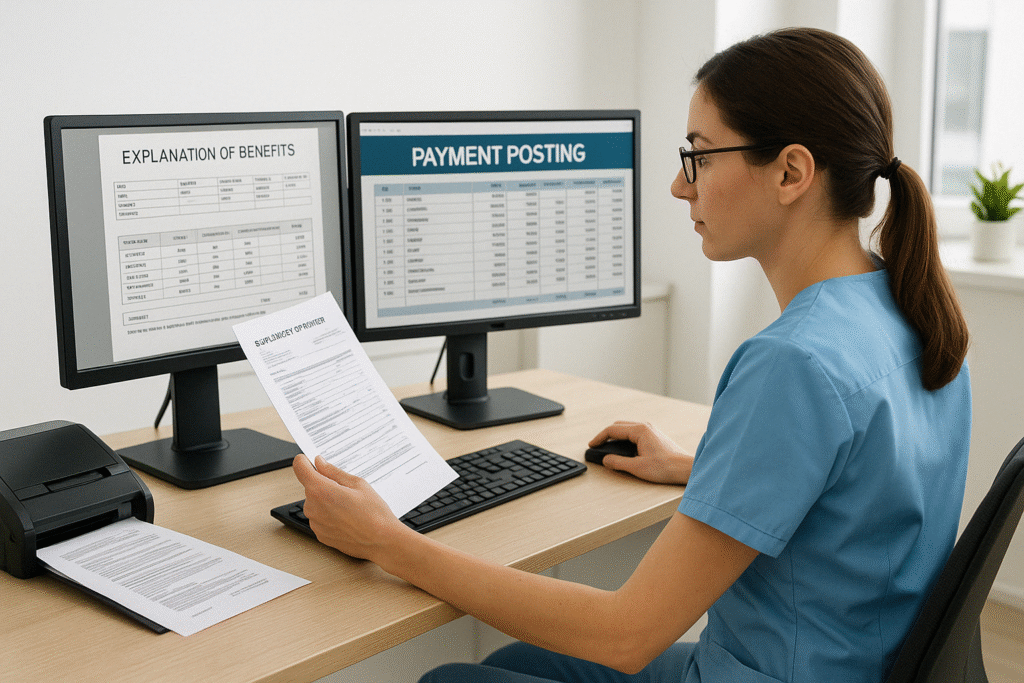
ERA & EOB Posting Process
Electronic remittances typically contain a high volume of payment transactions. The processing of ERA batches involves loading the files into the practice management system, processing exceptions from the batch run by making corrections using the functionality available. Payment data from scanned images of the Explanation of Benefit (EOB) document are captured line by line and posted to the respective patient accounts. ABC develops practice/physician specific business rules to ensure accurate payments, adjustments, write-offs, and balance transfers are posted correctly.